My Master’s program taught me about health systems strengthening. The concept is simple, clear, and ideal: you want to strengthen health systems. The harder part for me was the how. How do I do this? A health system is a large evolving enterprise comprised of many moving parts. What can I do to strengthen this from the outside?
Sitting five months into my fellowship, I realized I have witnessed this in action for the first time. It is complex, challenging, painful, yet in the end the system will be left more sustainable than how I found it coming in. This makes it all worth it.
In Rwanda, the public supply chain system goes from the national level, to the district pharmacies (DP), to the district hospital (DH) and health centers (HC). Partners In Health (PIH) used to have a parallel system. We would procure our own medicines and distribute them to hospitals and health centers in our catchment area. This weakens the public supply chain system as products on the National Medicines list could be obtained free from PIH or cost money from the district pharmacies.
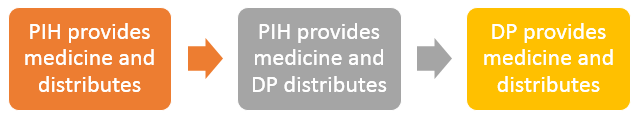
PIH began phasing our programs slowly from PIH dependent supply chain to public dependent supply chain. I see this process occurring in three major steps of which we have programs in different levels.
The first phase is PIH bringing the treatment to Rwanda. Our oncology program currently runs in this stage. PIH procures the medicines and distributes directly to our hospitals and cancer center. Now, this doesn’t strengthen the supply chain system too much, but it does bring in a new level of care to the health system that was not present before. Cancer can be treated in our facilities because of this step.
The second phase is PIH providing the medicine but the public system distributing it. Our non-communicable disease (NCD) program is in this stage. PIH procures the medicines, but we distribute it to the district pharmacies who then provide it to the hospitals and health centers. This allows the regular channels to supply the medicine even if the medicines come from PIH instead of the national level. The benefits of this are exposing the district pharmacies to the products and allowing natural distribution schedules to occur preparing them for when the medicine will come nationally and trickle down through this already set up distribution system. This prepares the DPs for when PIH will stop providing the medicine and allow the health system to take over. It begins the creation of sustainability that is not present in the first phase.
The third phase is PIH no longer supplying medicines and the public system taking on full responsibility for the adequate supply of medicine. Our essential medicine program is in this stage. At PIH we no longer carry essential products nor do we play any role in its distribution to our catchment area. The public system carries the entire burden for this section of medicines. Products are procured at the national level and trickle down to reach the health centers.
All three levels are very critical to the strengthening process. Bringing in new programs and slowly passing them off to the public system allows time for patients to start getting care and to ease the transition to PIH no longer being necessary in that subset of care. It is fascinating for me to see this play out and to see the transitions between long standing programs and new innovative programs. Essential medicines were the priority 8 years ago, but now PIH is no longer involved. The Oncology program only started a few years ago so it will slowly start to transition through the same phases. I am excited to be here and witness the gradual process PIH employs so that health care can continue thriving in Rwanda long after PIH leaves the country.